EXCELLENTTrustindex verifies that the original source of the review is Google. I had a wonderful experience with my treatment here. I came in with toenail fungus a couple months ago, had a series of laser treatments (plus integrating all of the other steps recommended by the doctor) and now my nails/feet are clear, and I couldn’t be happier. I took the LIRR from Bk to the officePosted onTrustindex verifies that the original source of the review is Google. Exceptional customer service and truly a professional team! Dr. Bhela explains each detail with confidence and set a game plan from the first visit. I would definitely recommend him to all!!!Posted onTrustindex verifies that the original source of the review is Google. If you are suffering from stubborn plantar wart, I highly recommended Dr. Bhela. He made a stubborn plantar wart that I had for 1 year finally gone after 3 months with SWIFT treatment. I highly recommended SWIFT for plantar wart. The staff was amazing and helpful with scheduling. Overall, I had wonderful experience at Restore Podiatry.Posted onTrustindex verifies that the original source of the review is Google. My experience with Dr Behla was great. Very knowledgeable, took care of my issue in one visit. I went to multiple doctors without any progression. Highly recommend him!Posted onTrustindex verifies that the original source of the review is Google. Dr.Bhela is very professional and detailed at getting results. I Had a great experience at Restore Podiatry and Laser center. Stop spending your money with over the counter ointments that just don’t work. For stubborn nail fungus you need to see a professional to rid yourself of it. Hot laser or cold laser is painless and you will definitely see the results you want spend the money the right way the first time around.Posted onTrustindex verifies that the original source of the review is Google. Dr. David Bhela in Hicksville NY , helped reduce my calluses in less than a month! Super professional, kind, and knowledgeable. Highly recommend!Posted onTrustindex verifies that the original source of the review is Google. Dr. Bhela is a great doctor who is very knowledgeable and helpful. He cares for his patients and you will find that out for yourself if you visit him! He has helped me a lot with my feet and I couldn’t be more thankful. He definitely gets my personal recommendationVerified by TrustindexTrustindex verified badge is the Universal Symbol of Trust. Only the greatest companies can get the verified badge who has a review score above 4.5, based on customer reviews over the past 12 months. Read more
Toenail fungal infections are widespread, impacting nearly one in five individuals. Known in medical terms as onychomycosis, these infections can affect people of all ages and genders and are very challenging to eliminate once it starts. Dr. Davinder Bhela, DPM, a foot and laser specialist, explains the underlying causes of toenail fungus, explores both conventional and natural treatment options, and shares practical tips for preventing these infections from occurring.
Toenail fungus often starts when the nail is damaged, injured, or loosened, creating an entry point for fungal organisms. These tiny organisms are present virtually everywhere, on both indoor and outdoor surfaces, constantly seeking a place to grow and multiply,” explains Dr. Bhela. “Feet, being warm, damp, and often confined inside shoes, create the perfect environment for fungal growth
Nail damage can result from repeated friction, such as that experienced during running or other sports, or from an accidental injury. Once the nail is compromised, fungi can penetrate beneath and between its layers, gradually taking hold. In more severe cases, the fungus may even reach the nail matrix, which is the area responsible for producing new nail growth.
Other factors that increase the risk of developing toenail fungus include:
Wearing tight-fitting shoes
Walking barefoot in damp communal areas like pools, saunas, or public showers
Poor circulation in the legs
A weakened immune system
Medical conditions like diabetes
In many cases, the earliest indication of a fungal nail infection is a small spot of discoloration—white, yellow, or brown—appearing beneath the nail’s edge. As the fungus progresses deeper, the nail can become thickened, brittle, crumbly, and noticeably discolored. In some instances, the infection may spread to nearby nails.
However, these symptoms alone don’t guarantee a fungal infection. To confirm, a small nail sample needs to be examined under a microscope to detect the presence and type of fungus. This testing helps the doctor decide on the most appropriate treatment plan, if treatment is needed at all.
For most individuals, toenail fungus is more of a cosmetic issue than a medical one, though it can still cause frustration and embarrassment.
If you’ve been struggling with toenail fungus, you may be wondering why it seems so stubborn and resistant to treatment. The answer lies in the way toenails are built and how the infection hides.
Toenail fungus usually settles under the nail plate or between the nail and the nail bed. Sometimes it grows on top, but most often it burrows underneath where it’s protected. Because toenails are designed to be tough and durable, they create a shielded environment that allows fungus to survive and multiply.
Unlike skin, toenails are not very porous. This means most medications—including creams or topical solutions—struggle to penetrate deeply enough to reach the fungus in effective concentrations. As a result, the infection often lingers despite treatment.
Toenails also have poor blood circulation compared to other parts of the body. Since blood carries immune cells that fight infection, your body has a harder time clearing toenail fungus on its own.
Nails are made of stacked layers of keratin. The fungus doesn’t just affect the surface—it can live between these layers or directly beneath them, making it even harder for treatments to fully reach the infection.
In more advanced cases, fungus can invade the nail matrix—the area where new nail cells are produced. When the matrix is infected, the fungus affects every new nail that grows, making treatment especially challenging.
The Bottom Line: Toenail fungus is tough to treat because it hides beneath strong, protective nails, resists topical medications, and evades the immune system. That’s why professional treatments—such as FDA-cleared laser therapy—are often recommended. These advanced options can penetrate the nail more effectively and target the fungus at its source.
The right approach to treating a fungal nail infection depends on both the type of fungus involved and how advanced the infection is. The first step is usually scheduling a visit with a podiatrist or healthcare provider, who can recommend the most effective treatment plan and help lower the chances of the fungus returning. Starting treatment early is important, since the sooner it’s addressed, the better the likelihood of success.
When the nail is only mildly affected and not yet thickened, the infection is often easier to manage. Depending on your case, some of the treatment options your doctor may suggest include:
One of the most common ways to treat toenail fungus is with oral antifungal tablets, typically prescribed for a course of around three months. These medications work by helping new, healthy nail grow in place of the infected one. While generally safe, they aren’t suitable for everyone since they can interact with other prescriptions and may carry potential side effects. Long-term use has been linked to liver concerns, which is why regular monitoring by your doctor is essential during treatment.
For mild to moderate infections, oral medications are successful in roughly half of cases. However, the effectiveness tends to decline when treating more advanced or severe fungal infections.
Topical treatments involve applying antifungal solutions or lacquers directly to the nail to eliminate the infection—often used alongside nail thinning or debridement to enhance absorption. The goal is to allow the medication to penetrate the nail plate and reach the fungus underneath, promoting regrowth of healthy, fungus-free nail tissue. When used alone, especially without concurrent oral therapy, the effectiveness of topical agents tends to be modest.
For example, efinaconazole, a newer FDA-approved topical solution, achieves complete cure rates of approximately 15–18% in clinical trials—evidence of its limited efficacy when used as a standalone method MedscapeWikipedia. While not exactly 17%, this figure is very close and reflects real-world outcomes. Other topical agents, such as tavaborole, show even lower complete cure rates (around 6–9%) MedscapeLippincott Journals. Ciclopirox, the older lacquer-based treatment, has complete cure rates as low as 5.5–8.5%—again underscoring the challenges of penetrating the nail effectively JCADMedscape.
When combined with oral treatments, topical therapies can play a valuable supportive role—helping reduce recurrence and aiding in overall nail recovery, especially in mild to moderate cases.
| Topical Agent | Complete Cure Rate (Standalone) | Notes |
|---|---|---|
| Efinaconazole | ~15–18% | Best current topical option; still modest efficacy |
| Tavaborole | ~6–9% | Lower efficacy; newer mechanism |
| Ciclopirox | ~5.5–8.5% | Long treatment time; less effective than newer options |
Laser therapy has become an increasingly popular option for treating toenail fungus, particularly for patients who cannot tolerate oral medications. Evidence shows that the 1064-nm Nd:YAG laser is especially effective. In one study, treatment with a long-pulsed Nd:YAG 1064-nm laser (combined with 40% urea to thin the nail) achieved a 95.8% negative culture rate just three months after therapy (onlinelibrary.wiley.com).
In another clinical trial, 80% of patients treated with long-pulsed Nd:YAG laser experienced mycological clearance, while those treated with topical terbinafine continued to show positive fungal cultures (laserandhealthacademy.com).
These findings indicate that Nd:YAG laser therapy can outperform topical treatments and, in certain cases, rival the effectiveness of oral antifungal medications—making it a strong, non-invasive treatment choice for onychomycosis.
A study by Zhang et al. assessed the effectiveness of the PinPointe™ FootLaser in treating onychomycosis. The results indicated that 53% of patients achieved significant nail clearance, with many experiencing over 50% improvement in nail appearance. This study suggests that the PinPointe laser can be an effective treatment option for toenail fungus.PMC
The study by Kimura et al. evaluated the efficacy of the Cutera GenesisPlus laser for onychomycosis. The findings revealed that approximately 70% of patients showed significant improvement, with many achieving over 70% nail clearance. This study supports the use of the Cutera GenesisPlus laser as a promising treatment for toenail fungus.
| Laser Device | Study Reference | Reported Success Rate | Study Design |
|---|---|---|---|
| PinPointe FootLaser | Zhang et al. | ~53% | Clinical Trial |
| Cutera GenesisPlus | Kimura et al. | ~70% | Clinical Trial |


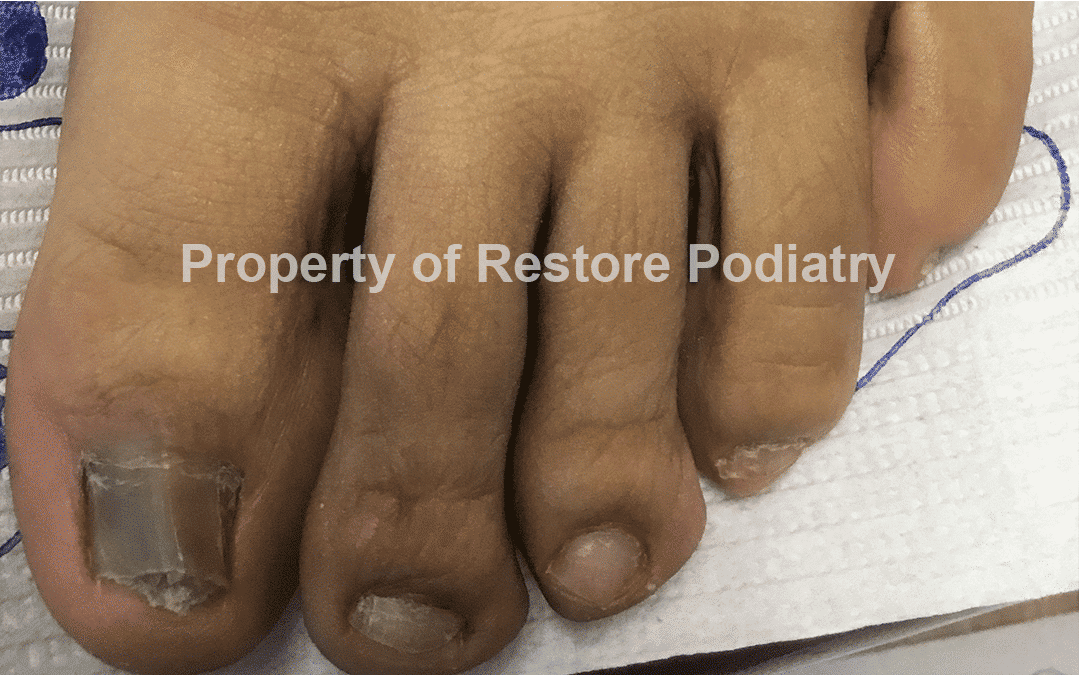
How?: “I think from skiing, wearing too tight ski boots”
Duration of Infection: 12 Years
Diagnosis: 75% Onychomycosis
Fungal Test Infection: Positive
Treatment Duration: December 2022 – May 2023
When treating toenail fungus with a 1064 nm Nd:YAG laser, an experienced podiatrist carefully adjusts several settings to maximize effectiveness while protecting surrounding tissue:
Wavelength – The laser uses a single wavelength of 1064 nm, which allows deep penetration into the nail and nail bed to target the fungus directly. The wavelength is crucial because it determines how deeply the laser energy reaches the infected tissue.
Pulse Duration – The laser delivers energy in very short pulses. Shorter pulses are effective at destroying fungal cells while minimizing heat damage to nearby healthy tissue.
Repetition Rate – This refers to how many pulses are delivered per second. The rate is tailored to your specific nail condition to provide sufficient energy to eliminate the fungus safely.
Spot Size – The diameter of the laser beam determines how much surface area is treated at once. Most spot sizes range from 1–10 mm, allowing the laser to cover the nail efficiently.
Fluence (Energy Level) – Fluence measures the amount of heat delivered to the nail. The podiatrist sets this based on the severity of the infection, ensuring enough energy reaches the fungus for effective treatment without harming surrounding tissue.
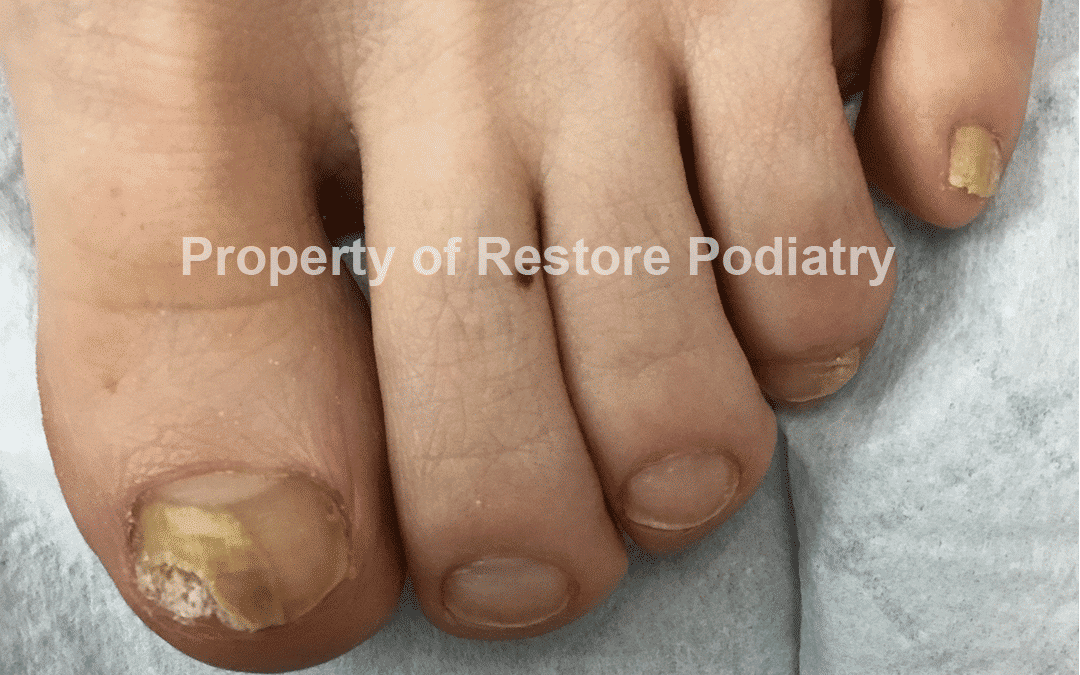
How?: “I think from nail salon”
Duration of Infection: 3 Years
Diagnosis: 90% Onychomycosis
Fungal Test Infection: Positive
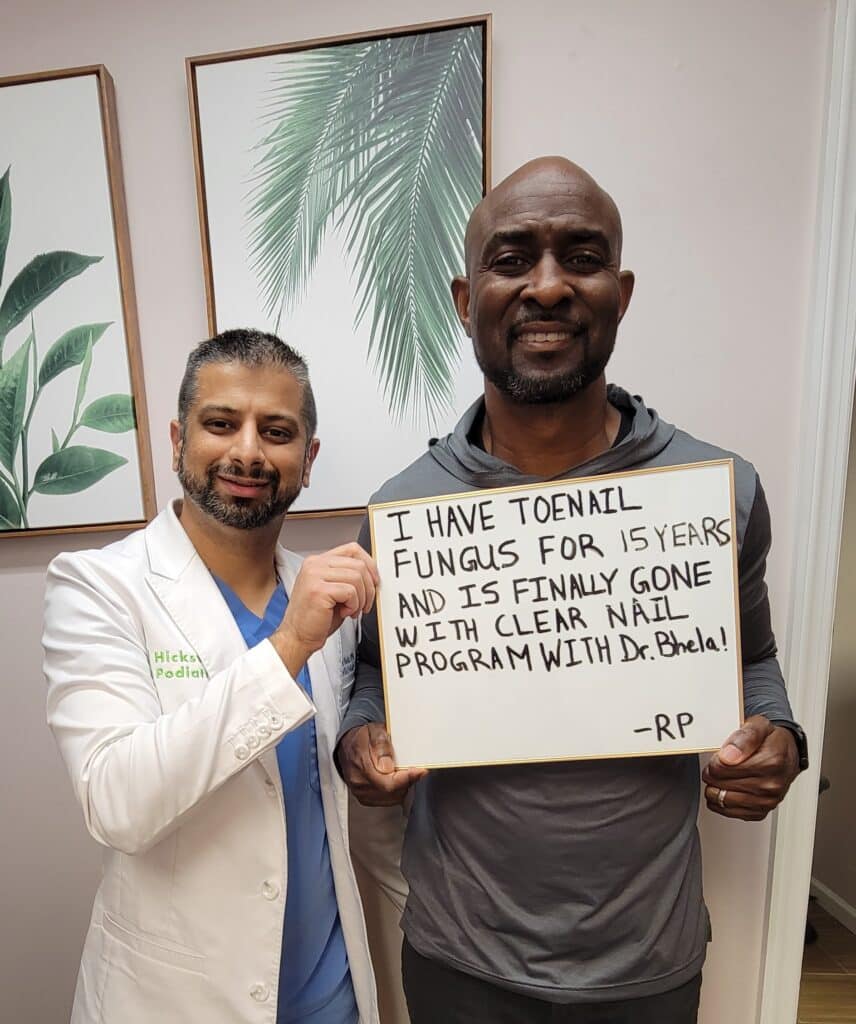
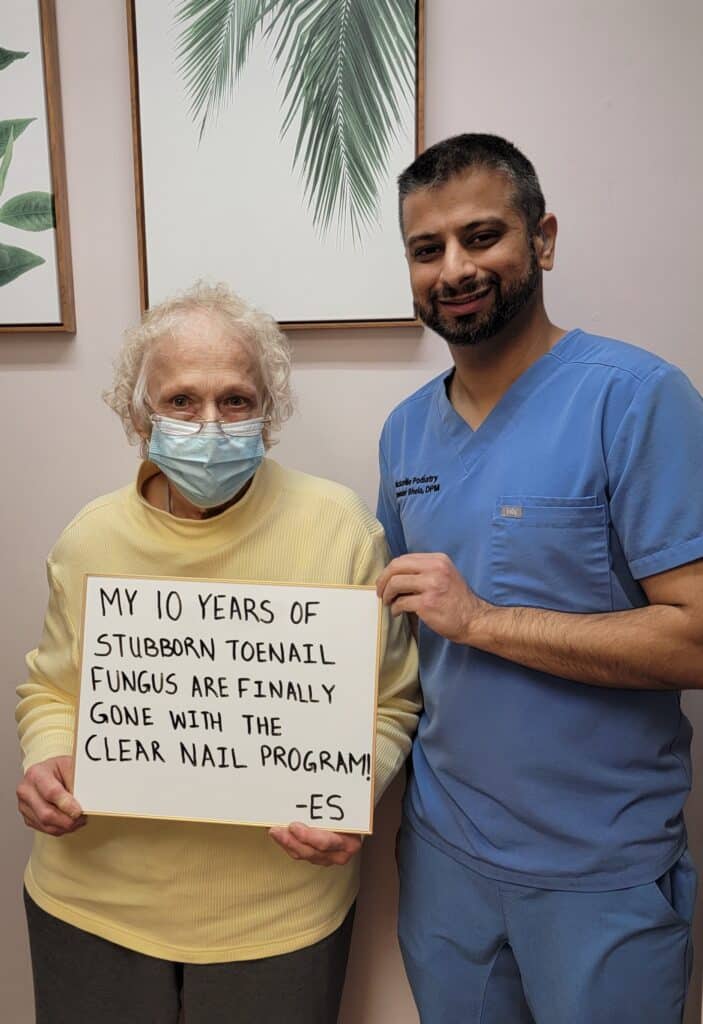
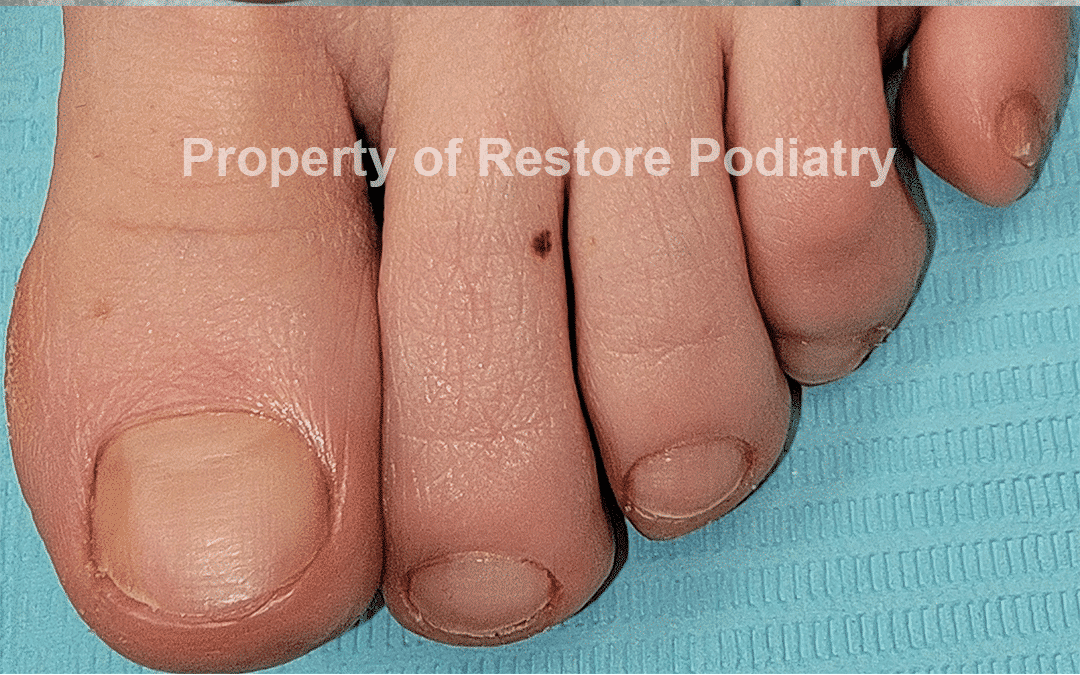
Clear nail program involves alternative treatment options that have no toxic medication, no sedation, and non-invasive treatment. Our unique combination of FDA approved treatment, backed by research, is the best way to deal with toenail fungus. By using a special laser with a combination of unique treatment, this treats toenail fungus at the highest level. However, you must first consult with your doctor and undergo an evaluation to know the right approach for you and customize your healing process. The treatment length usually differs per patient, but results can be seen within months. Our clear nail program has 90% success rate for all level of fungus severity from mild to severe toenail fungus.Our Clear Nail Program offers a safe, effective alternative to traditional toenail fungus treatments—without the use of toxic medications, sedation, or invasive procedures. This program combines FDA-approved technology with evidence-based care to target toenail fungus at its source.
Using a specialized laser along with a tailored combination of supportive therapies, we’re able to treat fungal infections at the highest level. Each patient begins with a thorough consultation and evaluation, ensuring the treatment plan is customized to their individual needs.
Treatment length varies depending on the severity of the infection, but visible improvement is often seen within a few months. With a documented success rate of up to 90%, our Clear Nail Program provides outstanding results for patients dealing with toenail fungus—from mild discoloration to more advanced cases.

How?: “From walking barefoot in damp public area”
Duration of Infection: 6 years
Diagnosis: Total Onychomycosis
Fungal Test Infection: Positive
Treatment Duration: February 2023 – July 2023
When other treatments fail to clear stubborn toenail fungus, surgical removal of the infected nail may be considered as a final option. The procedure is performed under local anesthesia, making it relatively quick and painless. After the diseased nail is removed, antifungal therapy is typically prescribed to help prevent the infection from recurring as the new nail grows back.
While this approach can be effective, studies show that the overall success rate is around 50%, meaning the infection may still return in some cases. For this reason, surgical removal is usually reserved for severe or resistant fungal infections.
While seeing a specialist is essential for persistent or severe cases of onychomycosis (fungal nail infection), starting with some home-based strategies may help manage symptoms and complement further treatments. Although many remedies show promise, most rely on limited or preliminary data—larger, controlled studies are still needed for conclusive evidence PMCPubMed. Below is a summary of at-home options, grounded in recent scientific findings:
Vinegar (Apple Cider or White): Soaking the feet in vinegar diluted with water (common ratios 1:2 or 1:3) lowers nail pH, creating a less favorable environment for fungal growth. While clinical trials are limited, many clinicians consider it safe as a supportive option.
Listerine (Thymol-Containing Mouthwash): Mouthwash soaks have anecdotal and small study support, likely due to thymol, eucalyptol, and menthol’s antifungal properties.
Tea Tree Oil (Melaleuca alternifolia): Several small trials suggest applying 100% tea tree oil twice daily may improve nail appearance and reduce fungal growth. One study showed results comparable to clotrimazole cream, though relapse is possible.
Lavender, Oregano, and Thyme Oils: These oils contain compounds (linalool, thymol, carvacrol) with demonstrated antifungal activity in lab tests, but robust clinical data is still lacking.
Propolis: A bee-derived resin shown in small trials to clear or significantly improve nail fungus in up to half of participants. Its penetration ability and antifungal properties make it a promising option.
Resin-Based Nail Lacquers: Natural resin varnishes, applied daily for several months, have produced moderate clinical improvements in observational studies.
Acidic Nail Polish (Acetic Acid Formulas): Some products using peelable acetic-acid–based lacquers showed comparable outcomes to medicated antifungal lacquers in early studies.
Iodine Tincture (2.5%): Case reports suggest daily application may improve appearance within weeks, though more research is needed.
Coconut oil contains medium-chain fatty acids, especially caprylic acid and lauric acid, which can disrupt fungal cell membranes. While strong clinical studies on nail fungus are lacking, in vitro data supports antifungal activity against Candida and dermatophytes. Many patients use coconut oil as a safe carrier oil for essential oils (like tea tree or oregano) or apply it directly to soften the nail and surrounding skin. Since it is well tolerated, daily use poses little downside, though results vary.
Baking Soda: Sometimes mixed into a paste and applied to nails to raise surface alkalinity, though antifungal benefits remain anecdotal.
Garlic: Contains allicin, which shows antifungal activity in lab settings, but topical use may cause skin irritation or burns.
Epsom Salt Soaks: Often recommended for comfort and reducing inflammation, though not proven to directly kill fungus.
Have any questions or concerns? Our team at Restore Podiatry is here to help! Reach out to us anytime, and we’ll be happy to assist you with expert advice and personalized care.